Understanding Aftercare Programs: A Critical Step Toward Lasting Recovery
Across the United States, aftercare programs are becoming increasingly recognized as a vital part of the recovery journey for individuals and families impacted by mental health challenges, trauma, and substance use disorders. While every recovery story is personal, common influences often include a combination of biological, psychological, and social factors. This article explores the significance of aftercare programs, drawing from up-to-date research and statistics to illustrate both the complexity of recovery and the hope that exists with the right support.
The Scope and Impact of Aftercare Needs
Mental health and substance-related conditions cut across age groups, economic backgrounds, and regions. Treatments such as Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) have been shown to significantly improve emotional regulation, behavioral control, and life satisfaction. In parallel, complementary practices like meditation are growing in popularity — with U.S. adult participation increasing from 7.5% in 2002 to 17.3% by 2022 — highlighting the growing shift toward holistic recovery methods that address both mind and body.
Physical and Emotional Repercussions
The consequences of untreated mental health issues and addiction extend well beyond the individual. Physically, prolonged substance use may lead to damage in key organs such as the heart, liver, and kidneys, while also raising the risk for infections. Mentally, individuals may struggle with anxiety, depression, and cognitive decline. These struggles often disrupt families, interfere with employment, and diminish overall quality of life. In the case of environmental disasters — such as fires, chemical exposures, or traumatic accidents — physical illness can be compounded by psychological trauma, leading to long-term health consequences that require sustained, compassionate care.
Recovery Solutions Rooted in Research
Effective aftercare is never one-size-fits-all. A successful recovery plan often blends multiple strategies. Evidence-based therapies like CBT and DBT provide a foundation for behavior change, while family therapy can rebuild communication and trust. Holistic options such as mindfulness meditation, yoga, and breathwork enhance self-awareness and reduce stress, and are particularly helpful for managing chronic pain or mobility issues. For many individuals, a combined approach that includes therapy, medication, support groups, and lifestyle changes proves most effective.
Navigating Resources for Long-Term Wellness
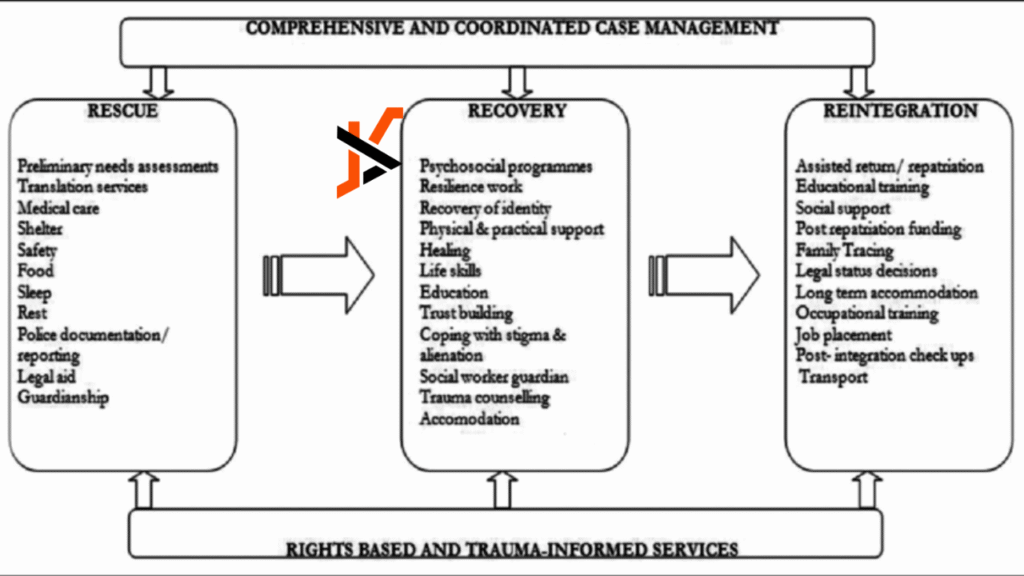
Accessing the right support is critical for recovery to be sustainable. Whether dealing with ongoing mental health struggles, the aftermath of addiction, or trauma-related challenges, professional guidance can make a meaningful difference. Aftercare programs offer structured services that help individuals transition from crisis to stability, reinforcing healthy habits, accountability, and self-empowerment. Connecting with knowledgeable providers, counselors, or peer mentors can be the turning point that transforms hope into progress.
Community Engagement and Policy Reform
Healing is not a linear process, and it doesn’t happen in isolation. A strong recovery system depends on accessible mental healthcare, community-based services, and supportive public policies. Practices like yoga and meditation not only promote individual wellness but also enhance collective resilience when integrated into schools, workplaces, and rehabilitation programs. Family-based interventions and culturally sensitive support services are especially effective in communities with historically limited access to care.
Legislation also plays a pivotal role. Nevada’s recent move to increase legal cannabis possession limits to 2.5 ounces reflects broader shifts in how substance use is regulated, aligning more closely with harm-reduction strategies. In parallel, traffic safety initiatives aim to reduce injury and death, acknowledging that risks related to addiction, distraction, and infrastructure neglect are deeply interconnected.
Genetics, poverty, trauma, and healthcare disparities are all significant contributors to mental health and addiction risk. For many, substance use begins as a coping mechanism for unmanaged pain, anxiety, or stress. Prevention, therefore, must extend beyond personal responsibility and address systemic barriers to wellness. Funding early intervention programs, increasing access to care, and integrating health education in schools can all reduce the long-term costs and suffering associated with addiction, injury, and neglect.
The Numbers Behind the Challenge
The statistics tell a compelling story. In 2023, only 7.9% of Americans with alcohol use disorder received treatment, even though 27.9 million people were estimated to have the condition. Meanwhile, insurers paid out $1.57 billion in dog bite liability claims in 2024 — a reminder that preventable harm exists in many forms. The American College of Physicians also now recommends yoga as a first-line approach for chronic low back pain, reflecting the growing trust in integrative care. These figures highlight the need for personalized, proactive care models that span mental, physical, and public health.
The Power of Group and Family Support
Group therapy offers a space for shared healing, allowing participants to relate to others facing similar challenges. Research shows that for many individuals, especially those with co-occurring disorders or social isolation, group therapy is just as effective as one-on-one counseling. These settings foster accountability, understanding, and emotional support. Complementing this with family therapy or grief counseling can help families rebuild and grow alongside their loved ones in recovery.
Public Safety and Holistic Health
The intersection between recovery and public safety is undeniable. According to the National Safety Council, more than 5,375 large trucks were involved in fatal accidents in 2023. With nearly 6 million motor vehicle crashes occurring annually in the U.S., injury prevention must be part of any public health conversation. From safer roads and better-designed infrastructure to responsible driving education, our approach to health must encompass mental, physical, and environmental well-being.
Creating a Healthier, Safer Future
When communities invest in research, treatment access, and preventative care, the benefits ripple outward. Early intervention, public education, and evidence-based policy reform are essential tools in reducing the long-term burden of untreated trauma, addiction, and injury. Whether through school-based coping programs, sober driving campaigns, or legislation that promotes health equity, we each have a role to play in shaping a safer, more supportive world.
Ultimately, the effectiveness of aftercare programs hinges on compassion, commitment, and collaboration. By combining individual therapy, group support, family involvement, and community action, we can break cycles of harm and build paths toward long-term recovery and resilience.